Glucose monitoring is an integral element of managing diabetes. The number of people with diabetes embracing cloud-based glucose monitoring technologies to keep connected with doctors while at home has significantly increased since the pandemic has made containment measures necessary. People with diabetes can use a smartphone to monitor their glucose levels by hovering it over a small sensor on the back of their arm. The conventional method of finger pricking has been replaced by this technology.
“It allows considerably greater potential for patients to be active participants in their care, even from a distance,” a Dunedin-based paediatric endocrinologist Associate Professor said of the cloud-based data sharing for diabetes. By being able to share their data so easily, the clinic continues almost as if there’s no disruption at all.
n keeping with the goal of easing diabetics’ lives, researchers at the Auckland Bioengineering Institute (ABI), New Zealand had successfully advanced a needle-free technology closer to reality, allowing individuals with diabetes to assess blood sugar levels without having to jab a needle into their fingertips. The researchers focused on needle-free jet injection, a new yet well-developed approach that involves delivering medicine directly through a high-speed narrow jet of fluid.
In a study published in the Journal of Diabetes Science and Technology, researchers from ABI demonstrated for the first time that a jet injector could be used to collect blood samples from humans, i.e., release enough blood for glucose sampling without the need for needles.
People with diabetes usually need to monitor their blood glucose concentration several times a day by pricking their fingers with a needle to release a drop of blood that is measured by a glucose metre, which reveals how much insulin is needed to keep their blood sugar stable.
Because of the high density of blood vessels on the fingertip, it is the best place to take a blood sample. However, the fingertips are delicate, and the pain, skin damage, bruising, and infection risk associated with regular ‘pricking’ has prompted increased efforts to develop needle-free blood testing methods for diabetics.
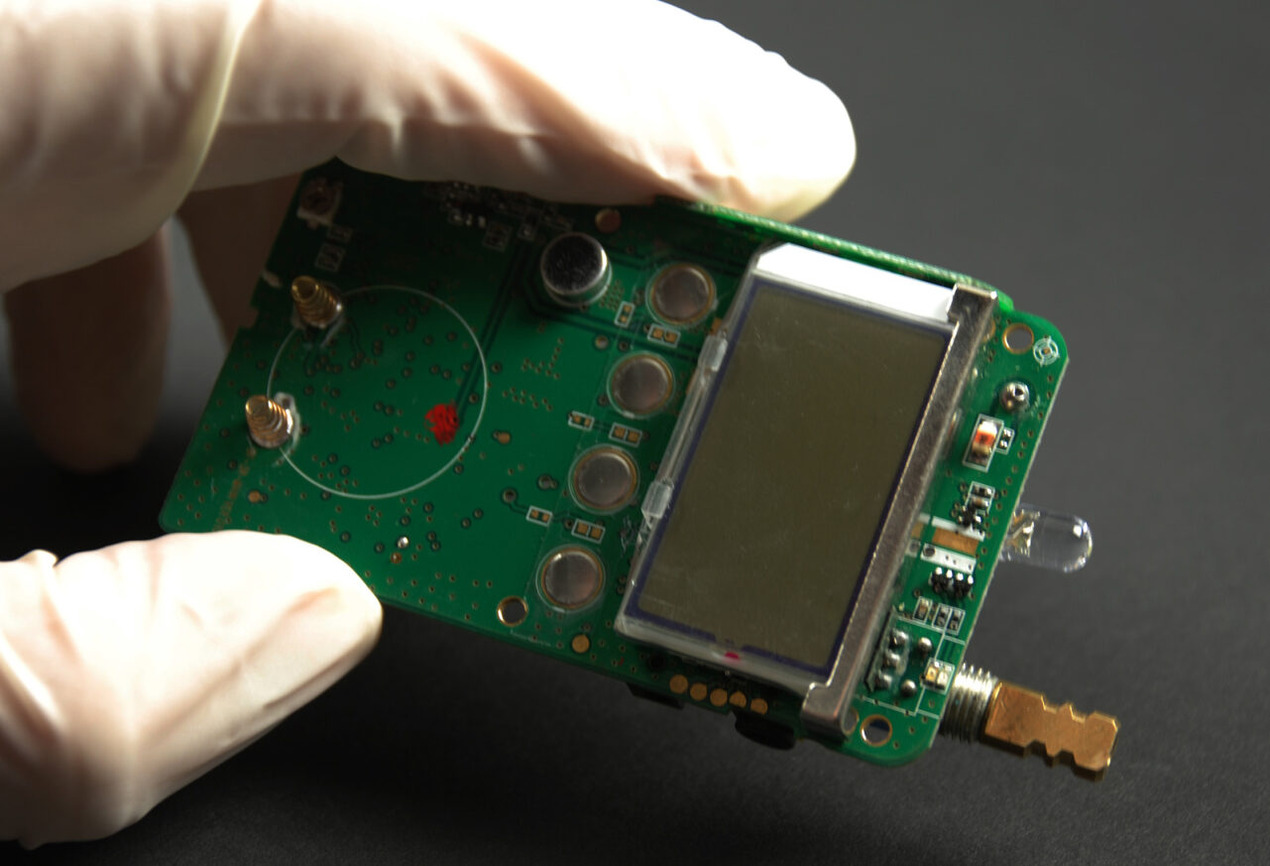
A jet injection is appealing for several reasons, including the apparent fact that many people dislike having a needle stuck in them. The ABI Bioinstrumentation Lab at the University of Auckland has been researching jet injection for years, including designing jet injectors for administering medications like insulin, nicotine, and as a local anaesthetic for dentistry treatment.
The researchers proved that the device may be used to pierce the skin with a small amount of harmless saline solution, releasing enough blood for glucose concentration measurement — rather than injection.
In addition, the team is now looking at whether jet injection can be used to not only release blood but also to suck back fluid. This would allow for the development of a nozzle that is even smaller. They have the know-how, having made the world’s first jet injection device that employs electric motors to pressurise the medicine, allowing for more precise control than the more conventional spring-actuated jet injector.
Further, claims one of ABI’s Bioinstrumentation Lab’s Professors, “Our technique is capable of both delivering and withdrawing fluid.No other jet projection technology has that capability.”
The development of a single lancet-free reversible technology that allows for both blood sampling and insulin delivery based on glucose measurement in one device is a long game, he says, but he believes the current research will contribute to the goal of developing a single lancet-free reversible technology that will allow for both blood sampling and insulin delivery based on glucose measurement in one device. “I hope that this research can help with that, as well as improvements in human healthcare, particularly in the management of diabetes,” the researcher added.
OpenGov Asia reported, the Auckland Bioengineering Institute (ABI) recently received Health Research Council (HRC) funding to conduct a pilot study in which they will test a portable temperature-sensing technology they developed to detect the early signs of foot complications in people with Diabetes 2. The prototype technology is a low-cost device designed for home-based monitoring, to detect early signs of foot complications.
It accomplishes this by measuring temperature asymmetries. According to research, temperature differences between our feet – for example, if the ball of the foot in the left foot is warmer than the same location in the right foot – are indicative of blood flow compromises. This can result in foot ulcers and, in severe cases, amputation. There is currently no method for objectively assessing temperature differences in our feet.
The device has been improved to be more user-friendly since its previous iteration. Patients are positioned on a platform that detects and maps minute temperature differences. The Research Activation Grant funding will allow the researchers to test the device by collaborating with an Auckland podiatry clinic and real patients.