|
Getting your Trinity Audio player ready...
|
Scientists from Washington University in St. Louis have created a sonobiopsy method to diagnose brain disease. The Sonobiopsy method employs ultrasound and microbubbles to momentarily breach the barrier, enabling brain RNA, DNA, and proteins to enter the bloodstream for analysis. While this technique was initially tested on animals, a recent study demonstrates its safety and viability for human use. This innovation may pave the way for non-invasive brain disease and tumour diagnostics.
Eric Leuthardt, MD, co-senior author and co-inventor of the technology, stated that Magnetic Resonance Imaging (MRI) drastically transformed brain disease diagnosis in the 1980s and ’90s, offering structural and functional brain imaging capabilities.
Leuthardt, the Shi Hui Huang Professor of Neurosurgery and a professor of neuroscience at the School of Medicine in biomedical engineering and mechanical engineering at the McKelvey School of Engineering referred to sonobiopsy as the third revolution, emphasising its molecular aspect. This innovative technique allows blood sample collection reflecting gene expression and molecular characteristics at the brain lesion site, essentially performing a brain biopsy without the associated risks of surgery.
Eric Leuthardt and Hong Chen, PhD, Associate Professors of Biomedical Engineering at McKelvey Engineering and Neurosurgery at the School of Medicine, developed the groundbreaking technique, focusing on multidisciplinary research to create engineered solutions for neurological diseases.
The technique employs focused ultrasound to target a brain lesion at a millimetre scale. Subsequently, microbubbles are injected into the bloodstream, travelling to the designated area and bursting, creating minuscule, temporary openings in the blood-brain barrier. These openings naturally close within a few hours, causing no lasting harm. Within this time frame, brain lesion biomolecules can exit the bloodstream, facilitating their collection through a standard blood draw.
Hong Chen, another Senior Co-author and co-inventor of the technology described this innovation as initiating a new field for brain-related conditions. It offers the capability to noninvasively and nondestructively access all brain regions, enabling the retrieval of genetic information about tumours before surgical procedures.
This information aids neurosurgeons in determining the best approach to surgery, helping confirm the nature of suspicious findings on imaging. Furthermore, it paves the way for studying diseases that typically don’t undergo surgical biopsies, including neurodevelopmental, neurodegenerative, and psychiatric disorders.
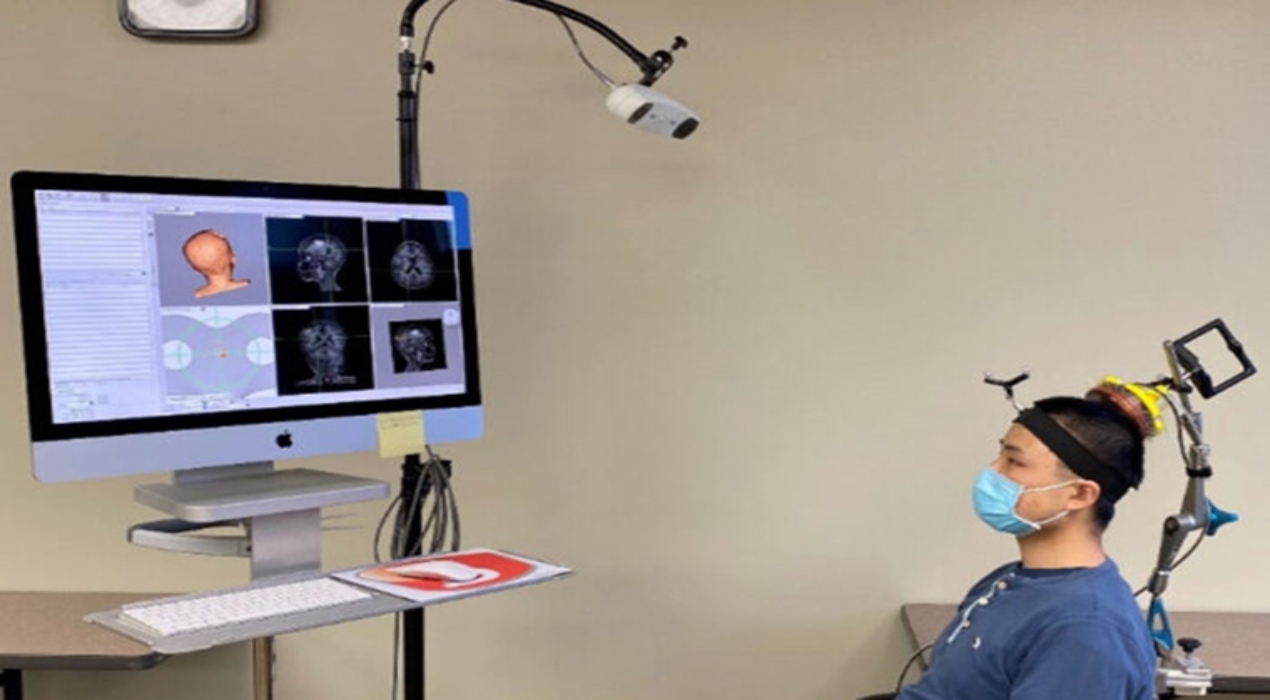
Initially, the researchers utilised a commercially available ultrasound device combined with an MRI scanner, a setup limited by cost and MRI availability. To streamline the procedure, Hong Chen’s team designed a portable, handheld ultrasound probe that could be attached to a stereotactic pointer commonly used by neurosurgeons for pinpointing brain lesions. This device was seamlessly integrated into the clinical workflow, requiring no additional training for neurosurgeons.
Eric Leuthardt emphasised the user-friendliness of this device, stating that it was efficiently utilised during the study in the operating room but could also be employed in a clinic or at a patient’s bedside in a hospital. He noted that this approach was a significant step toward making advanced diagnostics more accessible, enabling the examination of patients’ brains without needing a high-tech, multimillion-dollar scanner.
In their research, the team conducted sonobiopsies on five individuals with brain tumours using this device. Subsequently, the tumours were removed surgically following the standard care protocol.
The analysis of blood samples collected before and after sonication revealed that the technique increased circulating tumour DNA, ranging from 1.6-fold to 5.6-fold, depending on the specific type of DNA examined.
Circulating tumour DNA holds crucial information about genetic alterations in a patient’s tumour, which guides treatment decisions regarding the tumour’s aggressiveness. Notably, the procedure showed no signs of causing damage to brain tissue, affirming its safety.